AI healthcare booms as drug discovery and precision medicine take leaps forward
AI is transforming the healthcare industry.
As the technology evolves, the number of use cases within the sector continues to grow. Artificial intelligence now has a presence at almost every stage of the healthcare cycle.
AI is playing an increasingly important role in drug discovery. It is helping to triage patients and personalize treatment plans. It even has a part to play in carrying out surgery.
In this article, I explore all of that. But I also look at the trust and accuracy barriers that still need to be overcome before AI in healthcare can be truly ubiquitous.
Efficient AI as a driver of healthcare profits
Just like in other industries, the future role of AI in healthcare is to simplify existing processes. A paper in the National Bureau of Economic Research estimates that wider adoption of AI in the US healthcare system could generate annual savings of $200 billion to $360 billion.
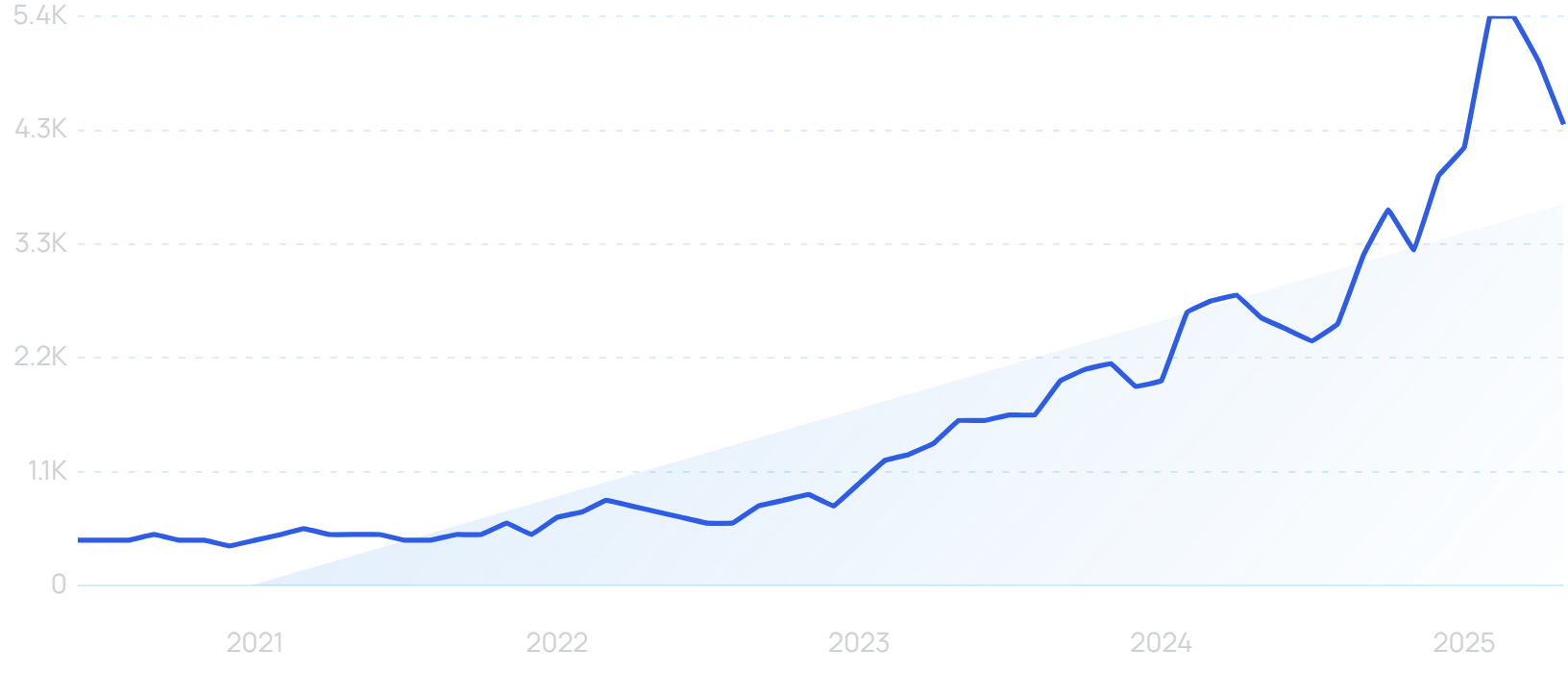
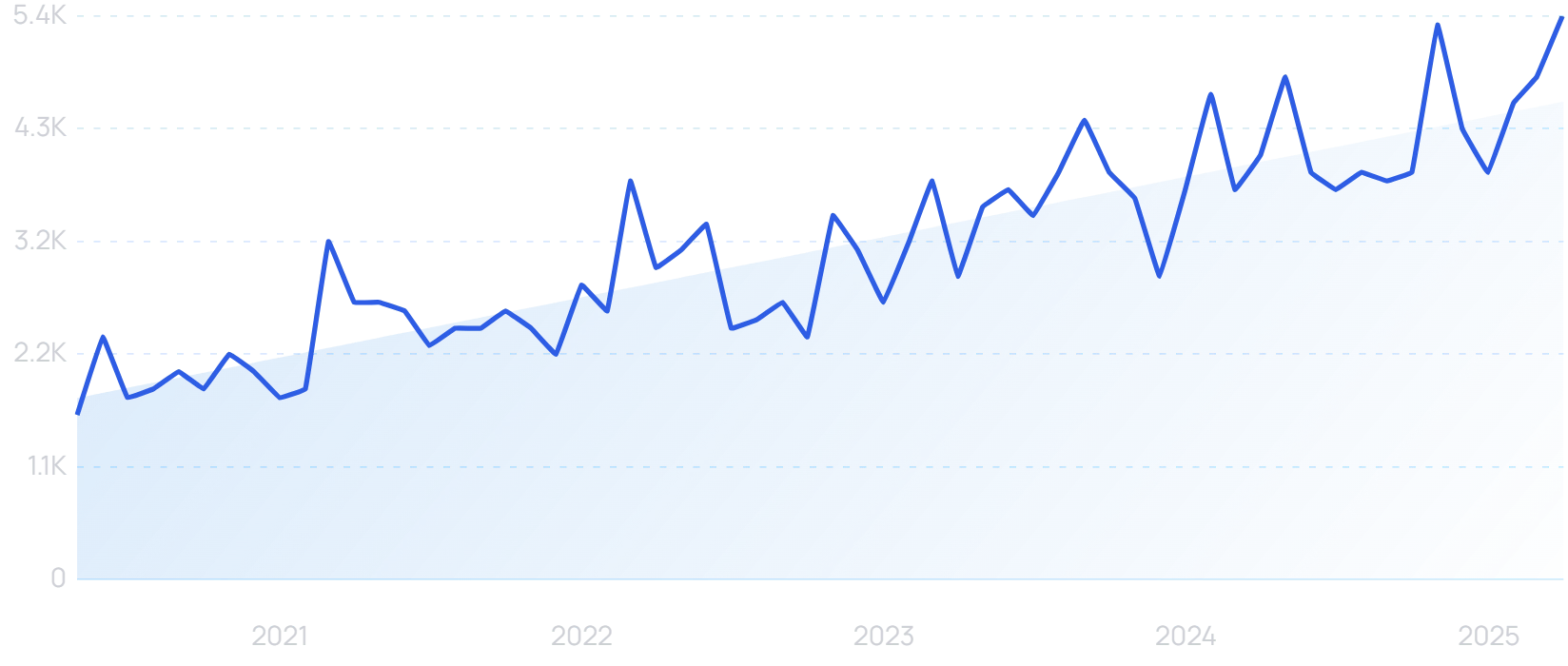
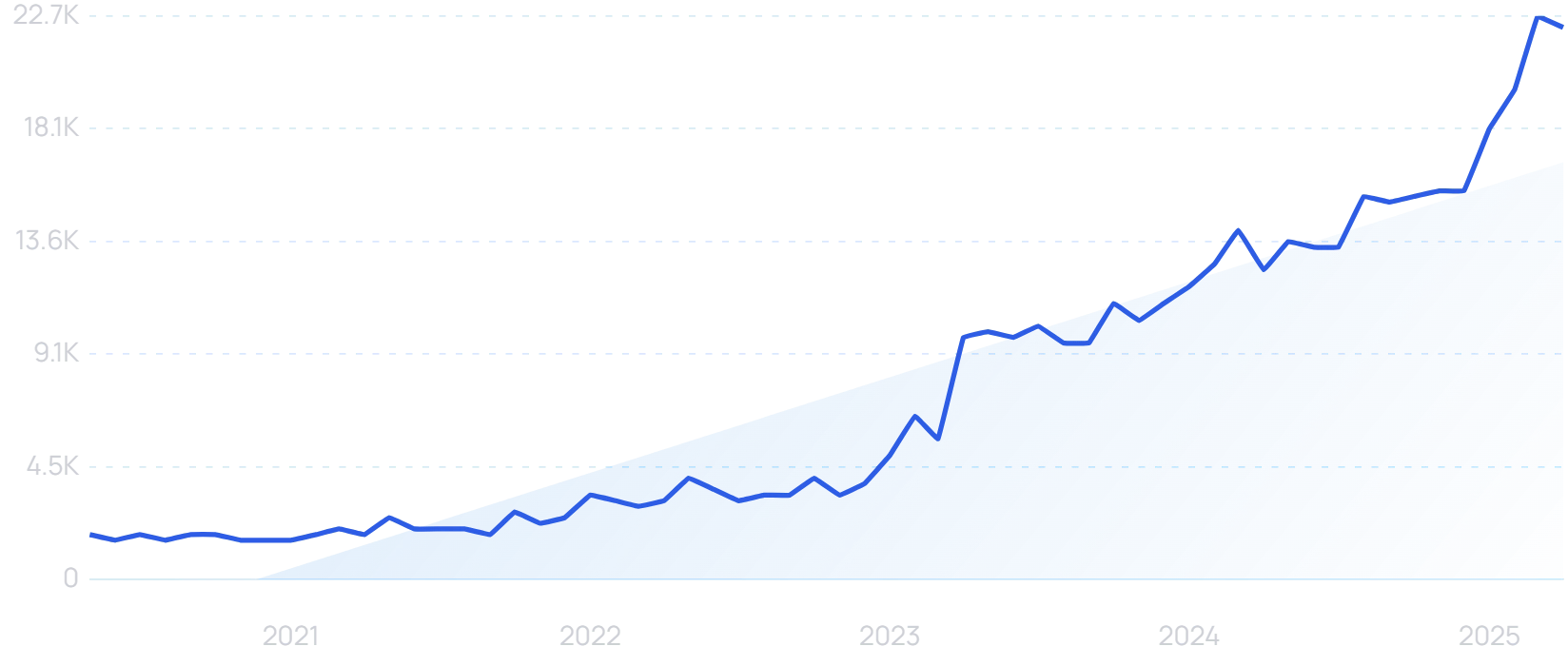
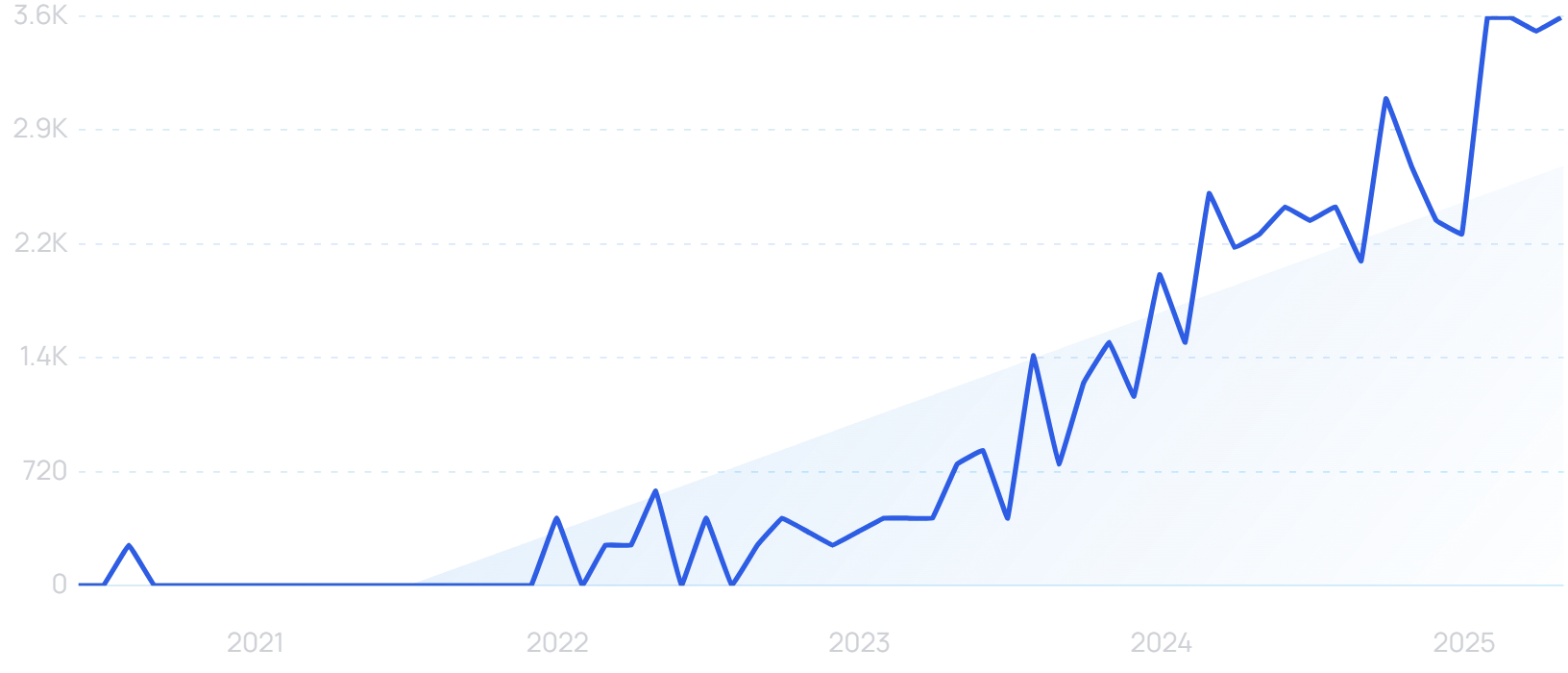
“Healthcare AI” searches are up 913% in the last 5 years.
Studies from the University of Oxford have found that no single healthcare occupation can be entirely automated — and that even in areas with high automation potential, automation desirability is often lower. Human contact remains a critical component of primary care.
Instead, AI is well-placed to significantly improve the efficiency of the jobs already being done by caregivers. Goldman Sachs estimates that 28% of work tasks performed by healthcare technicians and practitioners in the US could be automated.
And 92% of healthcare leaders believe automating repetitive tasks is crucial for addressing staff shortages.
As a result, the global healthcare automation market is projected to be worth $119.5 billion by 2033.
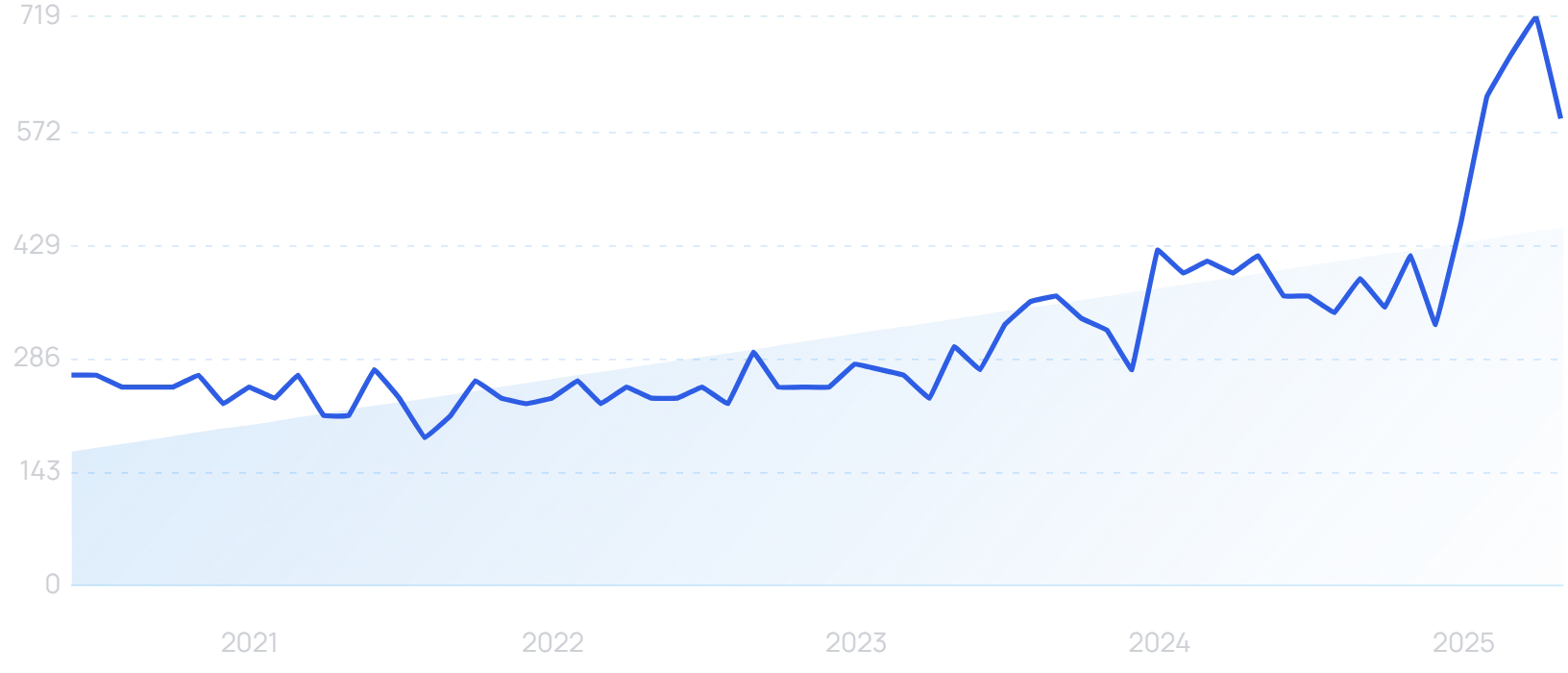
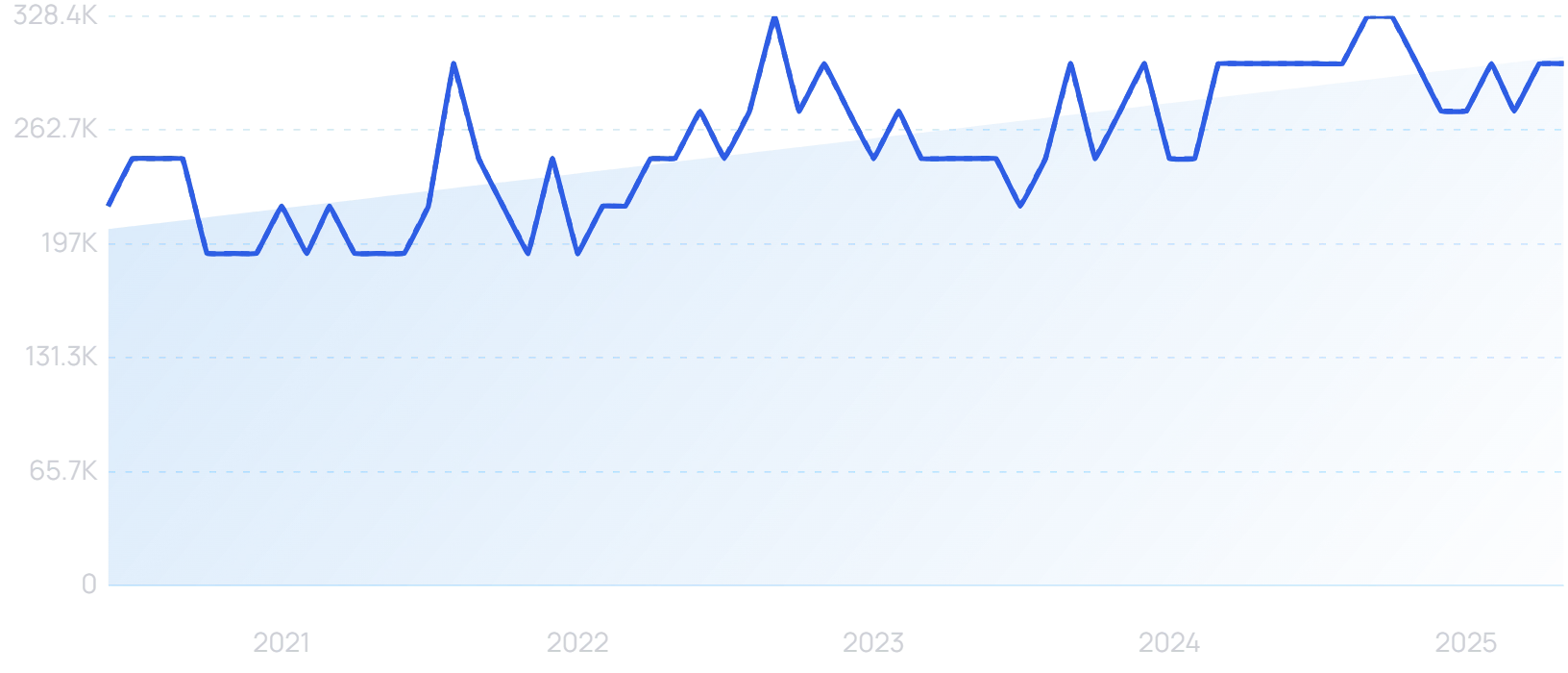
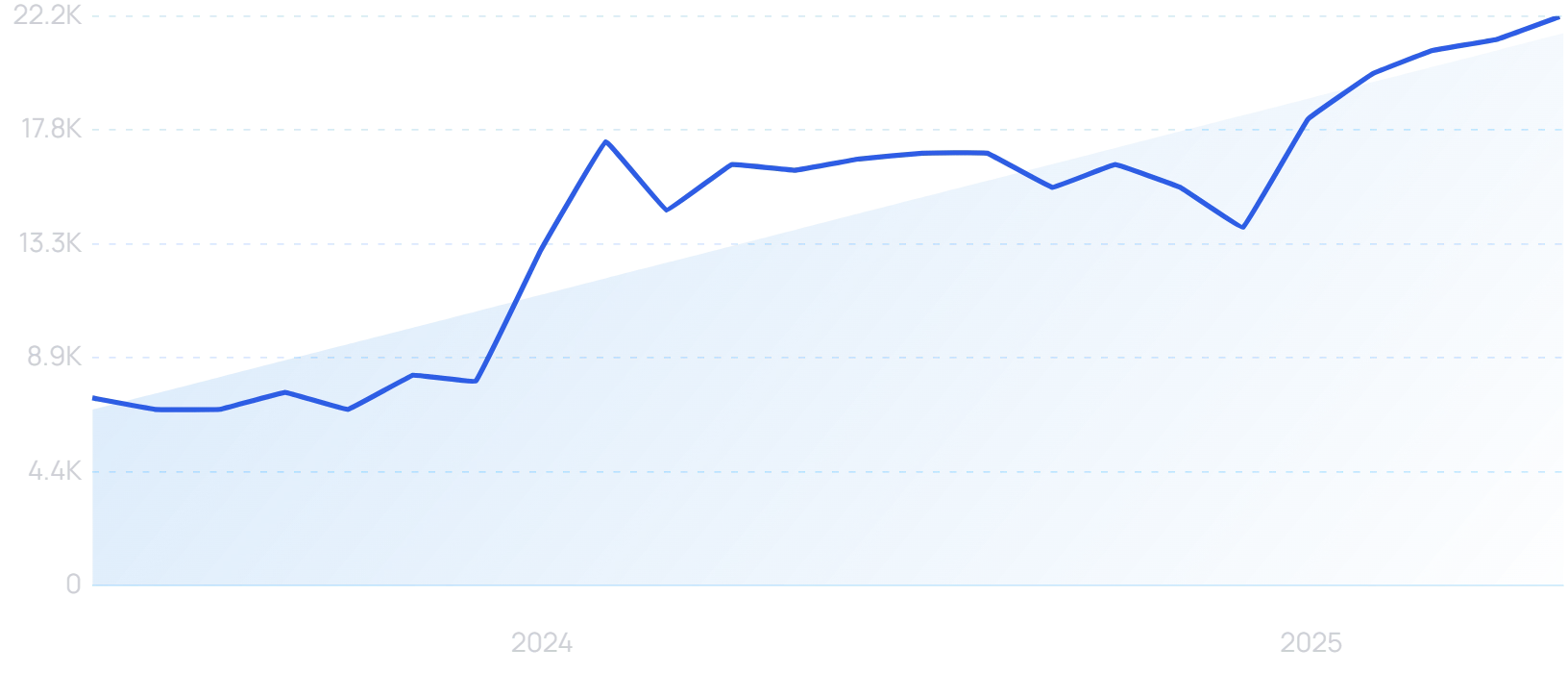
“Healthcare automation” searches are up 122% in the last 5 years.
Practitioners in critical care, internal medicine, neurology, and oncology spend an average of 18 hours a week on paperwork and administrative tasks. Using AI to automate some or all of that work would free up a significant amount of extra time to see more patients.
More than half of health leaders say their organizations have already implemented automation in clinical data entry, with a further 33% planning to do so within the next three years.
Among healthcare organizations that have already implemented generative AI in some capacity, more than half (54%) have already seen a meaningful return on investment.
And such is the rush to offer automation solutions to the industry, “healthcare AI” is now considered a hard keyword to rank for, requiring 268 high-authority referring domains and well-optimized content.
Build a winning strategy
Get a complete view of your competitors to anticipate trends and lead your market
Microsoft’s healthcare automation play
Microsoft paid almost $20 billion in 2022 to acquire Nuance, an “ambient intelligence” platform for the healthcare sector. It has since been incorporated within Microsoft Cloud for Healthcare.
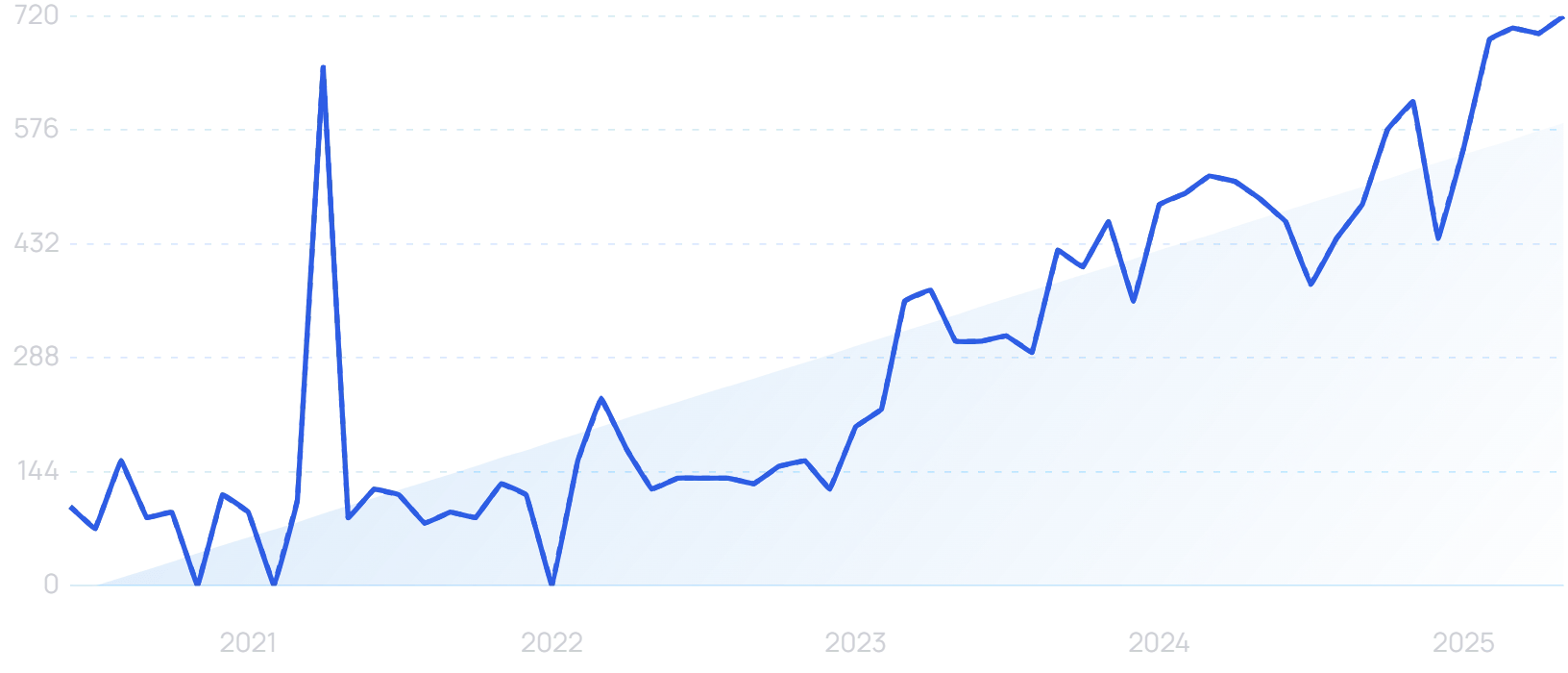
“Nuance AI” searches are up by 614% in the last 5 years.
In March, Microsoft released Dragon Copilot, an AI-powered voice dictation tool for healthcare professionals. It converts spoken summaries into specialty-specific notes, saving clinicians numerous hours.
Microsoft already has an extensive healthcare software suite. Its AI note-taking functionality therefore comes with the added advantage of integrating into a lot of medical organizations’ existing structures.
Last year, the majority of healthcare organizations said they considered Nuance when purchasing a clinical documentation solution.
And Microsoft is rolling out AI across its healthcare software, automating administrative tasks like patient scheduling.
Investment flows into healthcare AI
It isn’t just Microsoft betting big on healthcare AI.
Across all sectors, investors poured $56 billion into generative AI firms in 2023-24. In fact, AI startups claimed approximately 35% of all startup funding last year.
The healthcare sector has felt some of that benefit. Total venture investment in the industry grew by 17% in 2024, fueled by some big bets on healthcare AI.
In January 2025, Qventus raised a $105 million Series D round to develop “AI teammates” for medical personnel. Its technology seeks to reduce staff workloads through effective automation.
“Qventus” searches are up 90% in the last 5 years.
Through simplification and automation of scheduling, Qventus says it can utilize more than 50% of released operating room (OR) time blocks that may otherwise go unused. In total, it can unlock up to 9% more primetime OR capacity.
In March, Navina raised a $55 million Series C for its AI-enabled clinical intelligence platform aimed at primary care physicians. Goldman Sachs Alternatives led the round.
Innovaccer has also raised funds in 2025, completing a $275 million Series F. Its AI clears up patient data to harvest better insights, as well as saving clinicians “hours a day” by automating documentation.
In May, Rad AI brought its Series C round to $68 million. By automating the administration of follow-up care, its “Continuity” AI improves follow-up exam completion rates from 30% to over 75%.
AI unlocks precision medicine
While scheduling, note-taking and the less glamorous side of AI might have the most immediate impact on the bottom line for healthcare companies, there are also some exciting industry-specific applications of the technology that could ultimately change the landscape in more radical ways.
In particular, AI is already starting to unlock advances in precision medicine.
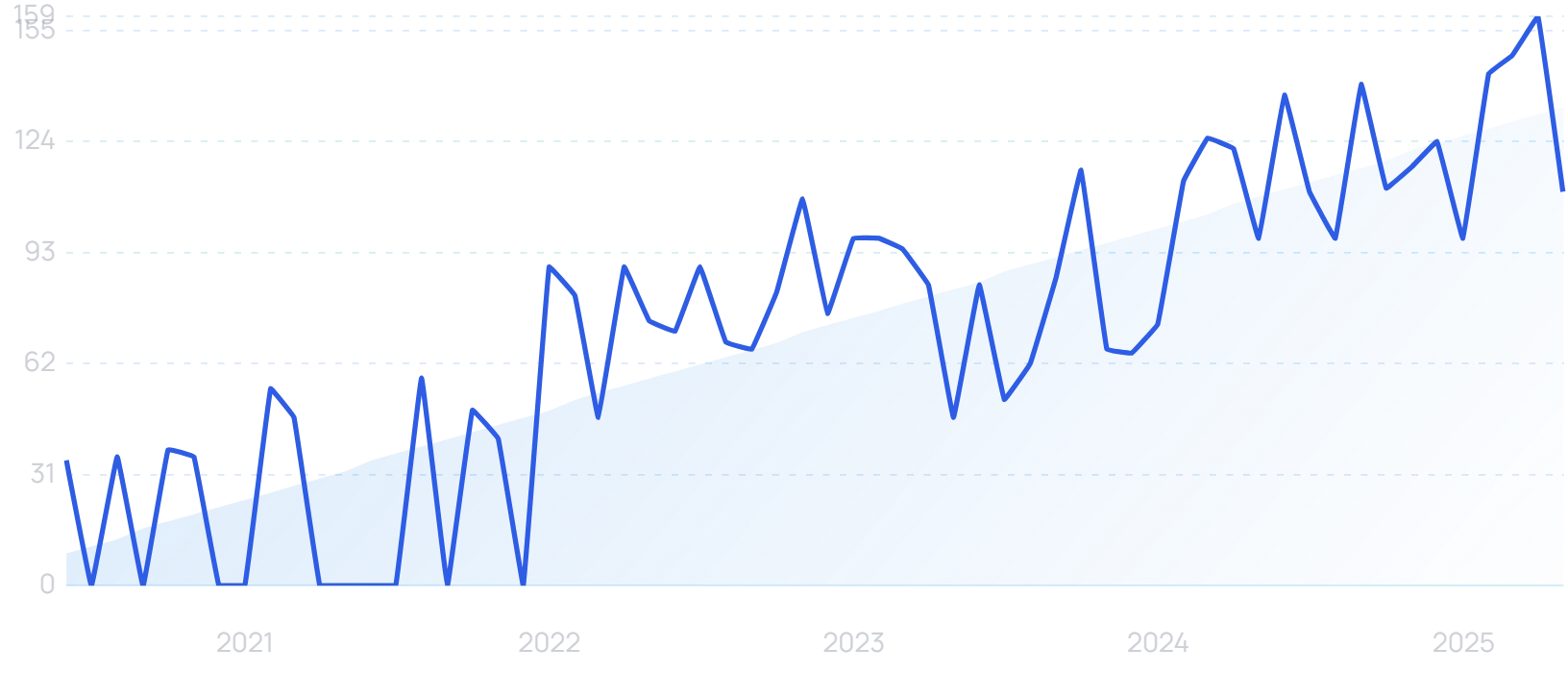
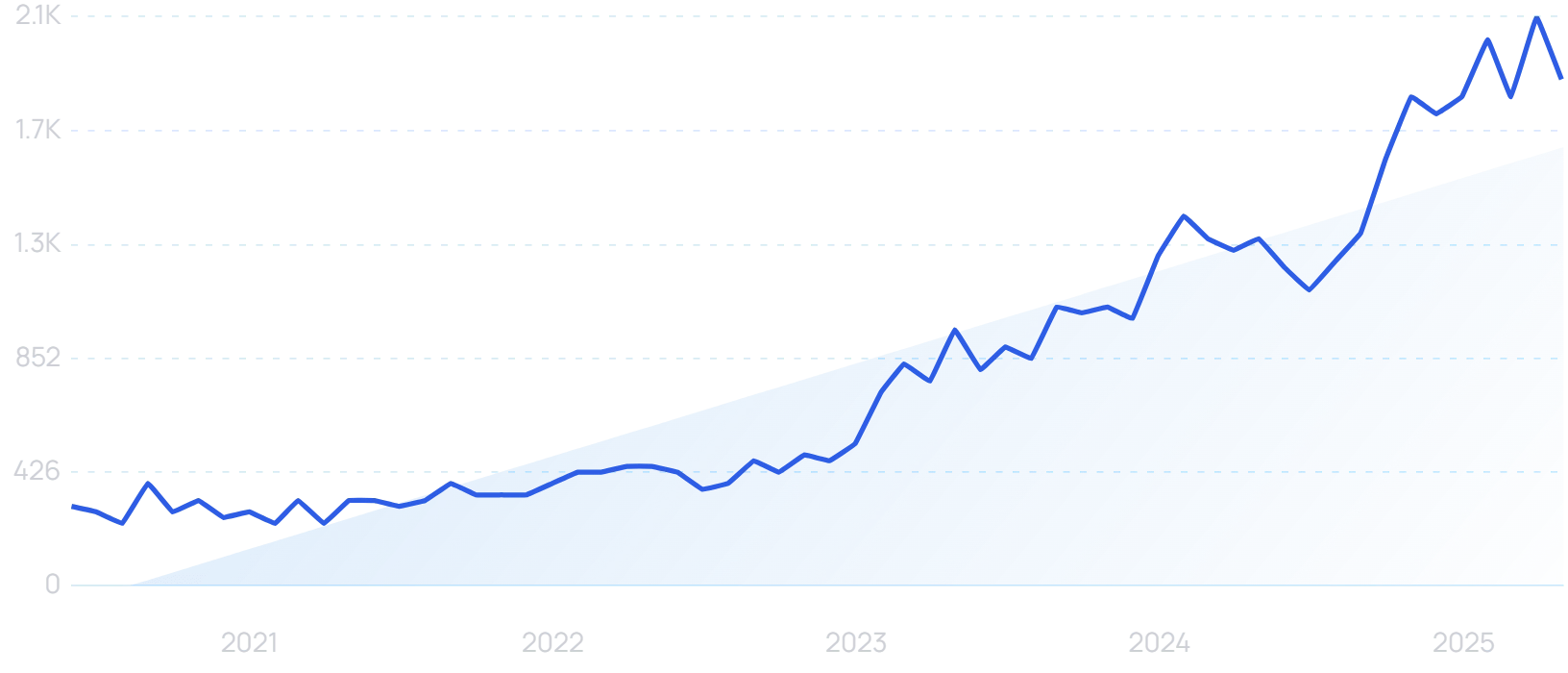
Searches for “precision medicine” are up 80% in the last 5 years.
Precision medicine involves treating patients based on their unique characteristics. While treatment plans have always been somewhat individualized, AI allows practitioners to be far more granular.
AI can process entire medical histories far more quickly and easily than a doctor or nurse. 97% of healthcare data currently goes unused, but digital transformation is beginning to harness this mine of information.
There’s the potential hurdle of what’s known as “healthcare interoperability”. This refers to the ability to access and share data between departments and organizations.
It’s a necessary step in using the full power of AI, but one which requires a certain amount of restructuring, as well as safeguards regarding patient privacy.
But in theory, AI can be used to quickly generate an extremely thorough patient profile. It can even draw from the “Internet of Medical Things” (IoMT), incorporating data from connected devices like smartwatches.
“IoMT” searches have risen by 91% in the last 5 years.
That data is only becoming more comprehensive as consumer tech companies embrace AI too. Apple is planning to add an AI coach to its Health app in 2026, clearly believing that it already collects enough health information to provide meaningful medical insights.
Apple’s AI can already help to detect falls, sense irregular heartbeats, and conduct sleep analysis, among other things.
Digital twins
Using all this data, AI can help to create a “digital twin” of a patient. This is a virtual recreation of the physical consumer.
Digital twins are highly useful for running simulations and calculating optimal treatment paths. For instance, they can help to ascertain ideal dosages and timing of medicines.
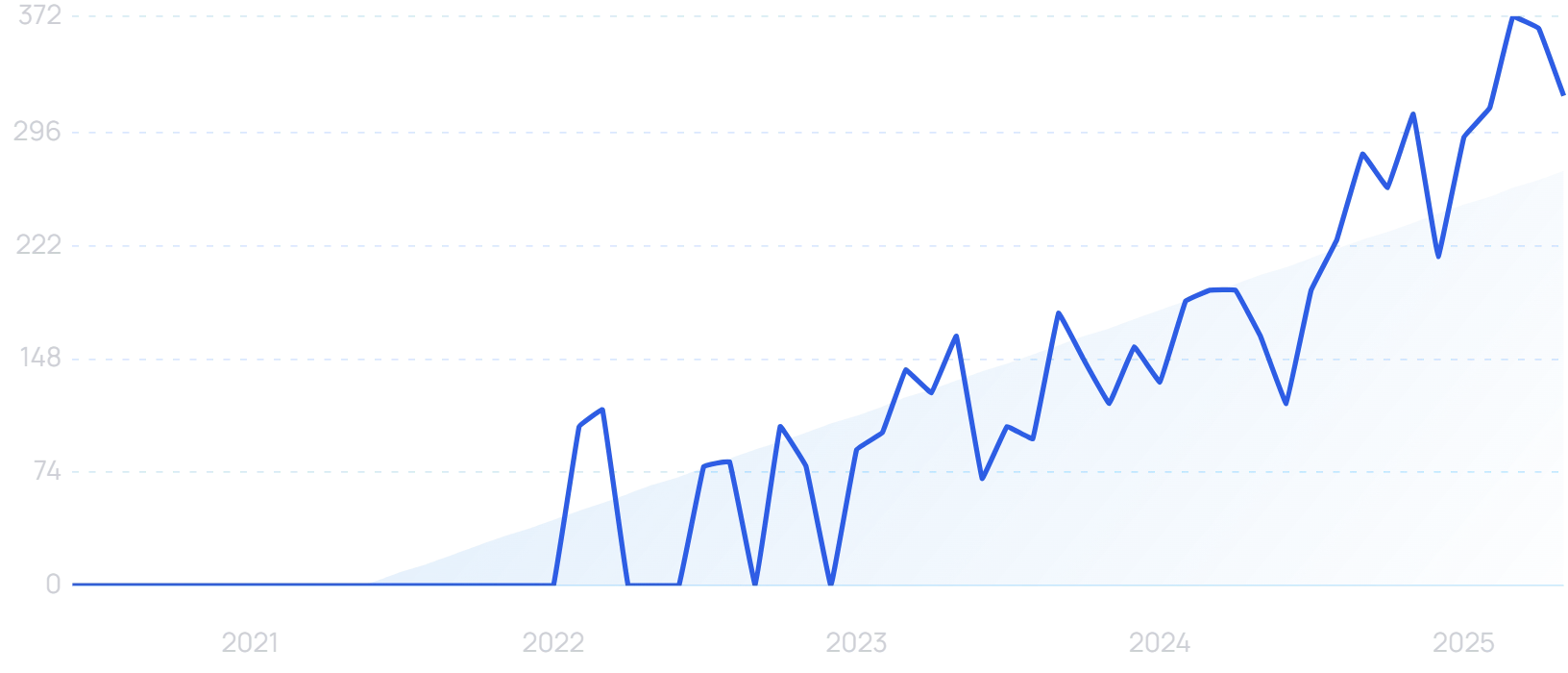
Healthcare digital twin” searches are still low, but are trending upward over the long term.
At Johns Hopkins, digital twins of patient hearts are being used to predict arrhythmias and adjust treatment accordingly. Simulated electrical waves are sent through the digital twin, allowing practitioners to see if they interact unusually with any scarring or damage — which can then be removed in real life.
These advances produce better medical outcomes. But they can also help to strengthen the trust between patients and healthcare providers.
The Deloitte 2025 US Healthcare Outlook study found that 43% of consumers are now using connected monitoring devices. If this data is taken on board and used to help devise a treatment plan, patients will feel as though they have been heard.
That’s a major challenge for the industry. In another study, 46% of patients reported “never or rarely” being asked for self-assessments of their conditions, which one participant described as “degrading and dehumanizing”.
AI transforms drug trials
Digital twins can be used in another medical context to radically change the process of drug trials. With AI helping to create a significant body of digital patient replicas, there’s a strong case for running simulations of new medicines on these virtual counterparts.
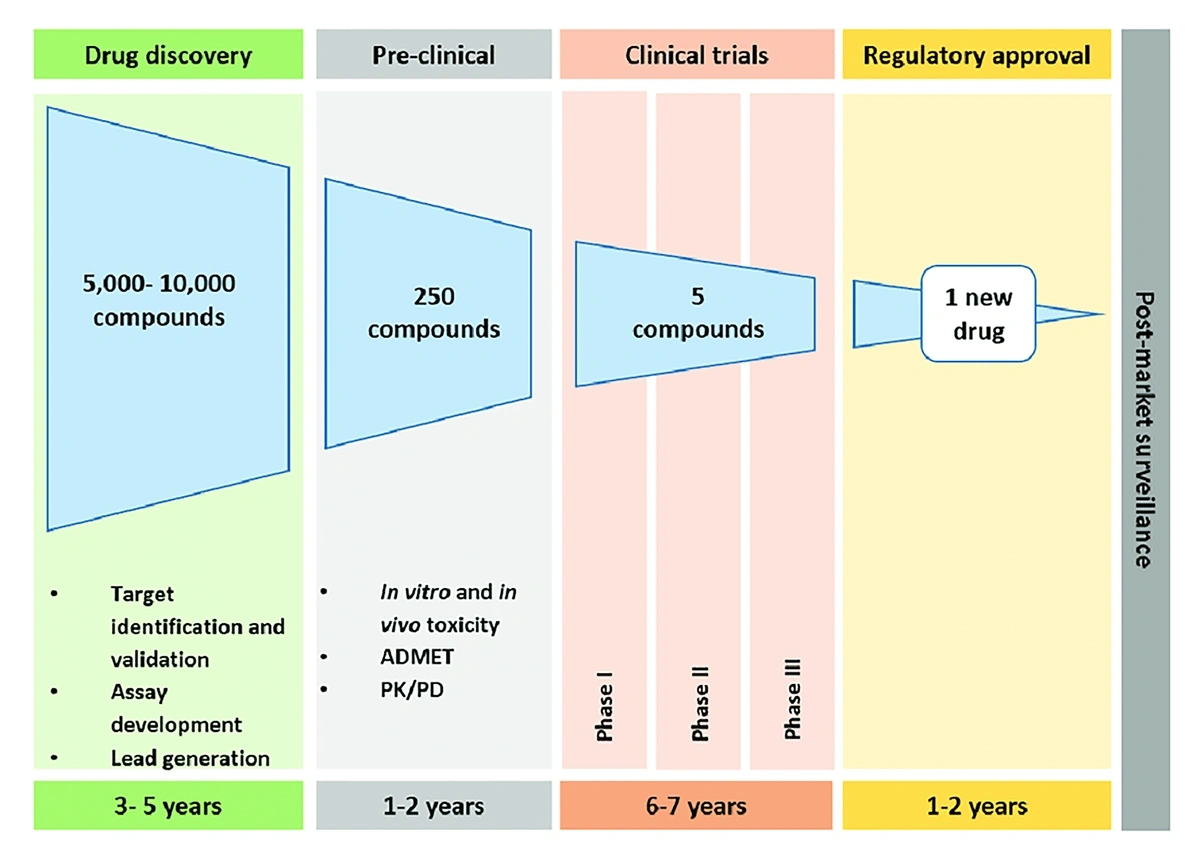
Most obviously, this removes the risks of adverse effects encountered in physical drug trials. But it also speeds up the process by orders of magnitude, with the timeline from initial discovery to full approval currently often 10 years or more.
One study placed the average drug approval pipeline at approximately 15 years.
Additionally, in classic trials, a drug could fail because the average patient response falls short of the trial’s target. By using digital twins, it is easier to isolate groups of patients where a drug is working particularly well, providing alternative routes to commercial and medical viability.
Drug companies are still testing on humans in the latter stages of development, and that’s unlikely to change any time soon. But Sanofi is using digital twins to effectively “skip” from a Phase 1 study to a Phase 2b study, with virtual patients used to establish optimal dosage.
AI drug discovery
Even before reaching the trial stage, AI has a massive role to play in drug development.
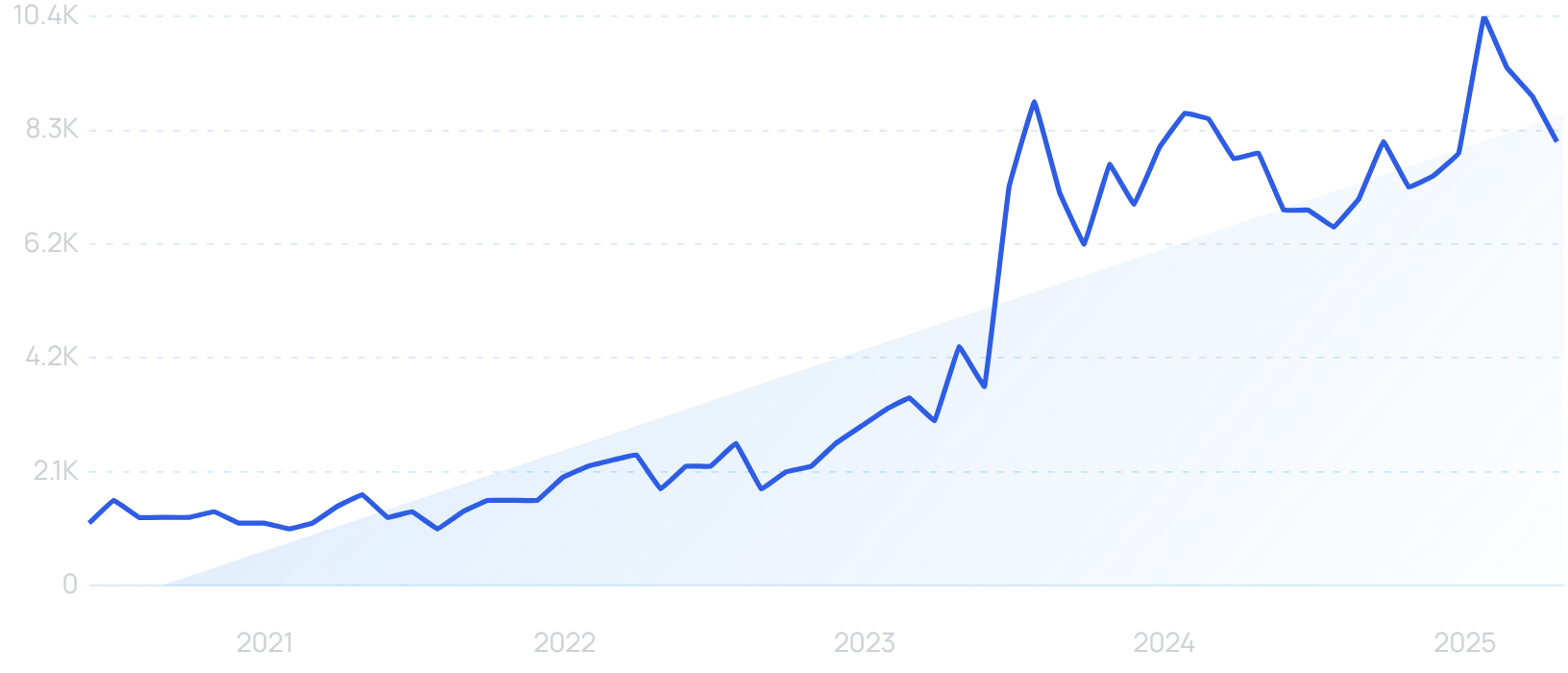
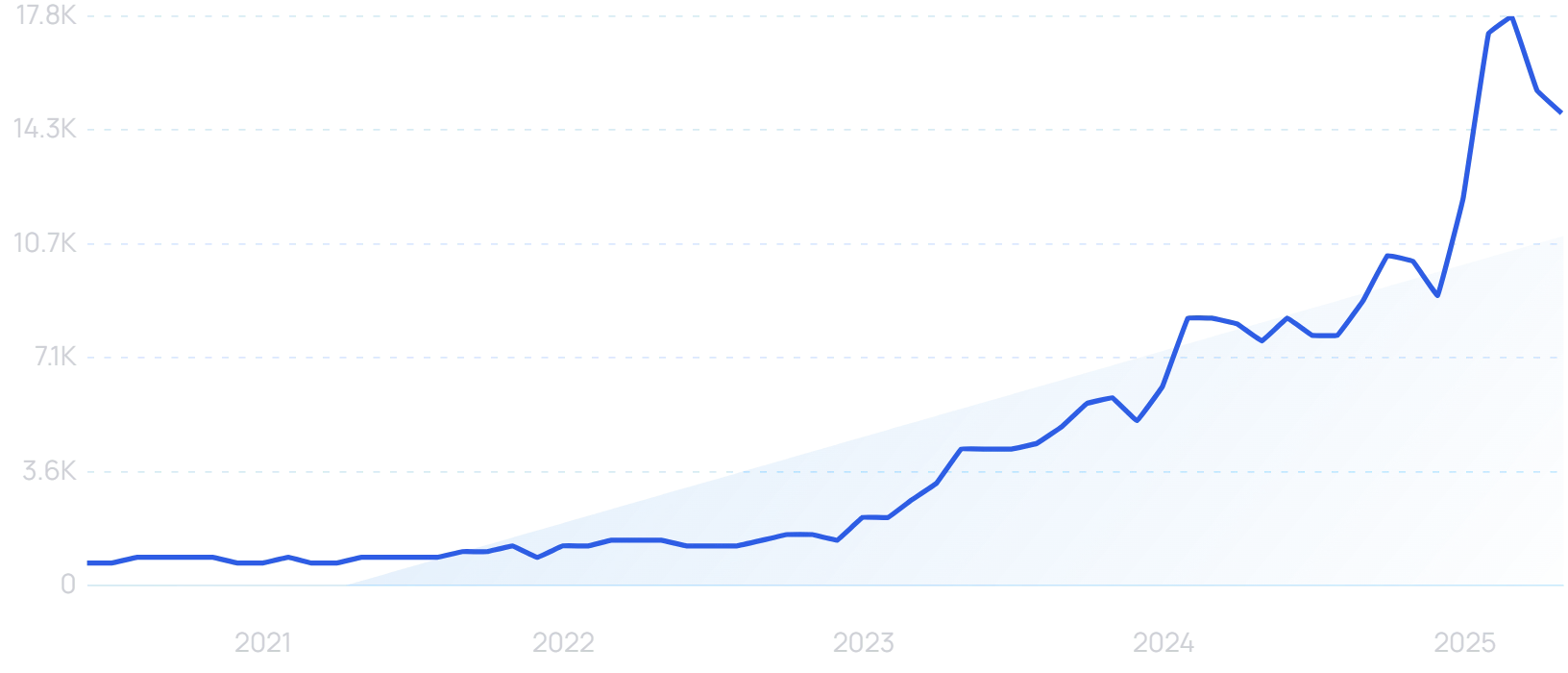
“AI drug discovery” searches are up 609% in the last 5 years.
AI can drastically enhance the drug discovery process. Trained on a vast array of relevant data, machine learning models can predict at a far earlier point which medicines are worth taking to the trial stage.
As well as acting as an early filter, ever-more advanced AI can also pose entirely novel drug suggestions.
Last year, 46 “AI-discovered” drugs reached phase 2 and 3 clinical trials. In total, at least 75 “AI-discovered molecules” have entered clinical trials.
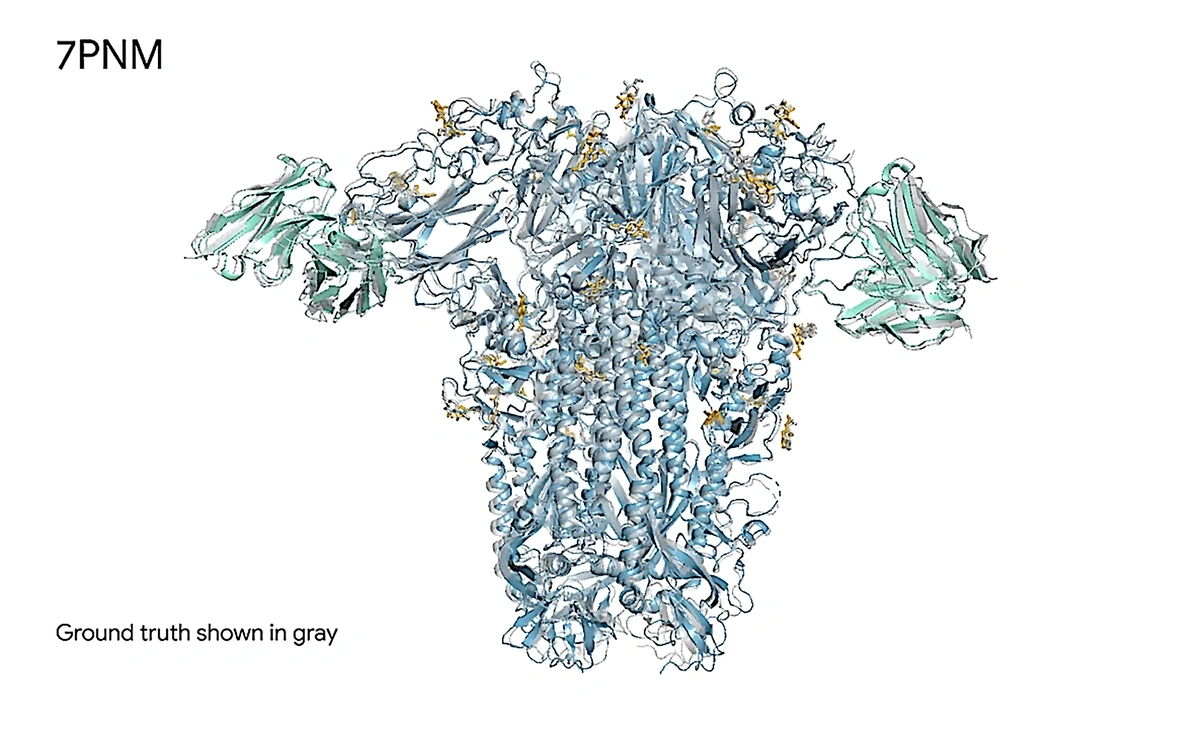
Google DeepMind and Isomorphic Labs have collaborated on AlphaFold 3. Drawing on a vast protein data bank, the AI model can accurately predict how combinations of these substances will interact on a molecular level.
AlphaFold 3 correctly predicted the true structure of a cold virus spike protein interacting with antibodies and simple sugars.
Isomorphic Labs is itself a drug discovery startup. And they and Google have since partnered with other pharmaceutical companies to make the AlphaFold 3 model available in drug development.
Deals with Eli Lilly and Novartis could be worth up to $2.9 billion, depending on the achievement of future milestones.
Using their own AI models, Insilico Medicine has taken a treatment for idiopathic pulmonary fibrosis to clinical trials within 18 months. The process would usually be expected to take 4 years.
Patient-Facing AI
AI is clearly already having a real impact on healthcare behind the scenes. But will patient-facing artificial intelligence ever become the norm?
AI doctors
There is already a vast array of “AI doctors” online.
“AI doctor” searches are up 1125% in the last 5 years
In one study, ChatGPT-4 scored an average of 90% when trying to diagnose a condition from a case report. Doctors acting alone scored 74%, while doctors aided by AI scored 76%.
Remarkably, another recent study even found that patients rated AI far higher than human doctors in terms of the empathy of their responses. ChatGPT was rated “empathetic” or “very empathetic” 45% of the time, compared to just 4.6% for physicians.
Even so, it seems unlikely that AI will be used this way in a clinical, institutional setting any time soon.
But Akido is using AI to tackle the shortage of human doctors.
“Akido” searches are up by 38% in the last year.
The startup says that the US population requires 3 billion doctor visits per year, with only 825 million currently available. It calls the physician shortage the single biggest challenge facing healthcare systems worldwide.
In May 2025, it raised a $60 million Series B round to develop ScopeAI as a solution to this problem.
ScopeAI visits are overseen by trained Medical Assistants, not doctors. The AI generates a preliminary diagnosis and treatment plan.
Akido says that its AI-guided healthcare visits have delivered a 5x increase in face-to-face time with patients.
AI robotic surgery
When discussing front-line medical automation, robotic surgery is never too far from the conversation. AI is impacting the landscape here as well.
“AI robotic surgery” searches are trending upward.
The “traditional” concept of robotic surgery is better referred to as robot-assisted surgery, with trained human surgeons guiding robotic arms to complete operations with greater precision. But what if the robotic equipment came equipped with AI?
Believe it or not, that is a question being asked in medical circles. A Johns Hopkins and Stanford University study trained a robot on hours of videos of skilled surgeons, after which it was able to execute the same surgical procedures with equal skill levels.
A senior author on the paper described it as a “significant step forward toward a new frontier in medical robotics”.
Robots are already used in one form or another in 4 million surgeries per year. The human role may well trend gradually from control to oversight.
As with the idea of AI primary care physicians, however, AI robotic surgery would need to become both more trustworthy and more trusted before becoming genuinely commonplace.
The need for trust
We’ve seen how AI can actually be a driver of trust when used to pursue more personalized, patient-driven precision medicine. But at least for now, the US public does not trust AI to play a front-and-center role in a healthcare setting.
According to one Deloitte study, 30% of consumers do not trust information provided by generative AI. 80% would want to be informed if a doctor was using AI in the medical decision-making process.
And the Deloitte Healthcare Outlook report was clear about the crisis of trust facing the healthcare industry. It’s an even higher priority for industry leaders than consumer affordability challenges.
Before AI can be widely used in any kind of patient-facing setting, healthcare bodies therefore need to ensure they have very robust AI governance frameworks.
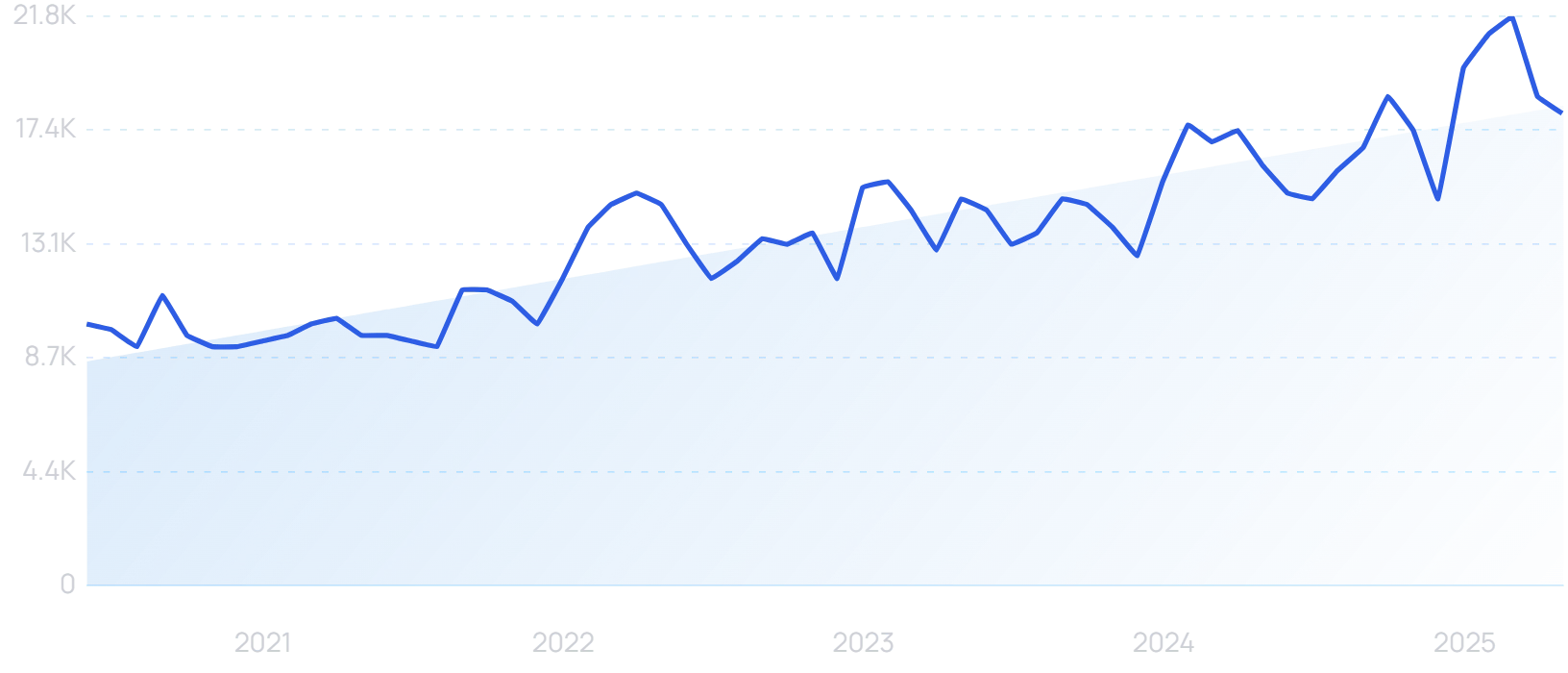
Searches for “AI governance framework” are up 8900% in the last 5 years.
An AI governance framework sets parameters for how AI will be developed and deployed within an organization. This is of vital importance in the medical profession, where there are questions of accountability to consider in the event of an AI misdiagnosis.
The World Health Organization has officially called for caution in the deployment of AI technology. It cites a list of concerns, including:
- The potential for bias in training data
- The risk of using private patient data to train LLMs
- The danger of convincing but medically inaccurate AI responses
The need for accuracy
Clearly, the need for accuracy in a medical setting is paramount. And while AI has beaten doctors in certain studies, models like ChatGPT currently remain susceptible to “hallucinating” plausible-looking but inaccurate information.
“AI hallucination” searches are up 203% in the last 2 years.
Human doctors might make a misdiagnosis. But these hallucinations introduce an entirely new class of potential error into the diagnostic process.
A National Institutes of Health study found that even when an AI model made the right final choice, it would often incorrectly describe medical images and give flawed reasoning behind a diagnosis. When allowed to consult external resources, physicians also diagnosed more accurately than the AI, especially on questions ranked most difficult.
AI needs to be more reliably accurate before it can be used on the front line in this manner. And perhaps even more critically, consumer trust in the technology’s accuracy needs to be built before such use cases are viable.
“Low-grade” clinical decisions
There are some clinical decisions AI can already make in its current form. In particular, the technology is proving useful in decisions one step removed from diagnostics.
A study at the University of California found that ChatGPT successfully identified the more urgent case in 88% of triage scenarios. Physicians made the right call 86% of the time.
The study noted that more tests would be needed before AI could be deployed responsibly in this manner in an emergency department setting. But across the healthcare industry as a whole, there is a definite movement toward automation of task prioritization.
36% of healthcare leaders have already implemented automation for the prioritization of clinical workflows. 41% plan to do so in the next three years, making it the largest single area of planned healthcare automation.
AIDOC has rolled out AI triaging software in over 1000 medical centers, including 7 of the 10 top-ranked US hospitals. Its software analyzes 3 million patients every month.
AIDOC’s AI triaging is already in use worldwide.
Away from triage settings, AI is already being used extensively to help analyze medical scans.
Of the 950 AI-enabled medical devices approved by the FDA, over 700 relate to radiology.
“AI radiology” searches are up 536% in the last 5 years.
Spectral AI is among the organizations working to apply AI to medical imaging. It specializes in scanning wounds.
Its DeepView technology predicts how wounds will heal, using scan information not visible to the human eye. Doctors can then use that information to inform treatment plans.
“Spectral AI” searches have grown 6700% in the last 5 years.
Spectral has received more than $7 million in US government funding.
Healthcare AI cybersecurity concerns
As in all areas of AI, advances in the medical sector are happening quickly. But it’s imperative that the security keeps up with the technology, especially in an area like healthcare.
Hundreds of millions of medical records are held on file in data centers across the US. In an ideal world, AI would play an important role in sifting through them and surfacing the insights needed to provide the best possible care for each patient.
But that data is highly sensitive, and highly vulnerable. Last year, a hack on Change Healthcare exposed the data of 190 million patients.
Since 2009, protected health information of almost 850 million patients has been exposed through data breaches.
It’s therefore unsurprising that more than 50% of healthcare decision-makers cite security concerns as the biggest roadblock to scaling the implementation of AI.
“AI cybersecurity” searches are up 1950% in 5 years.
Moreover, 72% of healthcare organizations are concerned about the security threats posed by advancements in AI. In particular, connected smart devices are considered easy access points for hackers.
This is a hurdle that needs to be overcome before AI can have a truly transformative effect on the healthcare industry.
Healthcare leaders must invest in AI to drive growth
AI is here to stay, and its use cases will only increase as the technology becomes more sophisticated. In terms of immediate applications, there’s a vast amount of administrative automation still to be done, and the healthcare industry is no exception.
As for specifically medical applications of AI, there are areas where the healthcare industry can already make use of the technology, notably in precision medicine, drug discovery, triage, and medical imaging.
And perhaps most importantly of all, the healthcare industry must work to build trust with patients. The growing use of AI within the sector makes this even more vital, and even more challenging — but when used responsibly, the technology can help to reinforce trust rather than undermine it.
Stop Guessing, Start Growing 🚀
Use real-time topic data to create content that resonates and brings results.
Share
Newsletter Signup
By clicking “Subscribe” you agree to Semrush Privacy Policy and consent to Semrush using your contact data for newsletter purposes
Written By


James is a Journalist at Exploding Topics. After graduating from the University of Oxford with a degree in Law, he completed a... Read more